Table of Contents
- Message from the Ombudsman
- Executive Summary
- Introduction
- Definitions
- Methodology
- Initial File Sample Review
- Second File Sample Review
- Findings: Inequitable Wait Times
- Findings: Opportunities for Needs-Based Triage
- Findings: Consequences of Delays
- Findings: Communication and Transparency
- Conclusion
- Footnotes
Message from the Ombudsman
I am pleased to publish my report Meeting Expectations: Timely and Transparent Decisions for Canada’s Ill and Injured Veterans. It focuses on the most common complaint my Office hears from Veterans: the length of time it takes to get a disability benefit decision from Veterans Affairs Canada (VAC).
The frustration and increased stress that this causes Veterans and their families must be eliminated. They deserve to know when a decision can be reasonably expected. If it will take longer than VAC’s 16-week service standard, they deserve to know why it will take longer and when their revised decision date will be. Both their mental and physical health care needs often depend on it.
What is especially worrisome to me is that our review suggests that not all groups of Veterans are treated equitably. Women wait longer than men; Francophone applicants wait longer than Anglophone applicants. Any differences in wait times for decisions should be based on need. All Veterans deserve timely decisions, regardless of factors such as language and gender. Discrepancies also exist in the way the Service Standard Start Date, or the date the “clock starts ticking”, is established, and under what conditions health care expenses incurred while waiting for a decision are reimbursable. As well, if a Veteran dies while an application is in process, their application may be withdrawn because VAC does not have the authority to allow such payments if there is not a spouse or dependent child.
Compounding these inequities is a growing backlog. That is why I encourage the Government of Canada to act on the seven recommendations in my report. They are supported by evidence-based findings and will enable VAC to better meet the needs of all Veterans and their families in a more timely manner.
Guy Parent
Veterans Ombudsman
Executive Summary
The most common complaint the Office of the Veterans Ombudsman (OVO) hears from Veterans is the length of time it takes to get a decision from Veterans Affairs Canada (VAC). Media has repeatedly covered the backlog of files, yet Veterans continue to voice their frustration about unreasonable delays.
Eliminating these delays is important. It is unfair to make Veterans and their families wait unreasonably for compensation to which they are entitled, especially when a favourable decision can also provide access to needed health care benefits. Furthermore, delays can mean unmet service-related health and financial needs and frustration for those waiting without any idea of when a decision can be expected.
To study this issue, 1,000 disability benefit first applications were analyzed, on-site visits with VAC staff were conducted, and all available internal and external documents that provide staff with instructions on processing and adjudicating applications – everything from legislation to business processes – were reviewed.
The analysis suggested that VAC quickly processes applications submitted by Veterans with World War II or Korean War service, as well as applications prioritized due to medical risk or financial distress. The majority of all other disability benefit first decisions, however, took longer than the established 16-week service standard – sometimes much longer.
When files were reviewed for trends, three patterns emerged:
- Inconsistencies in how certain groups of Veterans were treated:
- Francophone applicants waited longer than Anglophone applicants, on average.
- Delays were longer for women compared to men.
- Because of discrepancies with how the Service Standard Start Date – or the date the “clock starts ticking” – is determined, Veterans with less need may see their applications move forward in the queue before others.
- Disability benefit decisions made under the Pension Act provide better access to treatment benefits. For example, health care expenses incurred while waiting for a decision are reimbursable going back 90 days prior to the date of application, while those who fall under the Veterans Well-being Act only receive coverage on the date of decision. The backlog worsens this inequity. Delays mean some Veterans must pay for their own treatment while they wait or forego it altogether.
- Veterans and their families are treated unfairly when the Veteran dies while an application is in progress and they do not have a surviving spouse or dependent child. Current legislation does not permit VAC to pay disability benefits to an estate in these circumstances. Delays make this situation even more unacceptable. It is not fair that, due to delays outside the applicant’s control, there may be instances when an application dies with the claimant.
- A lack of prioritization for those who may be at risk for having unmet health needs:
- VAC automatically prioritizes applications submitted by elderly Veterans. As members of a vulnerable population, this helps to ensure they have no unmet health needs.
- Other Veterans can request a faster decision when they have an unmet health need or when experiencing financial distress. However, this process is not advertised and there is no way to know if everyone who needs it makes the request.
- Others with potential unmet health needs are not tracked or prioritized. For example, those about to transition out of the military.
- A lack of transparency and communication throughout the process.
- Due to inconsistencies in how Service Standard Start Dates are determined, turnaround time performance is not accurately reported or easily understood.
- Veterans are not given enough information about the status of their application, when they can reasonably expect a decision, or the reason for the delay.
Based on the findings, the report makes seven recommendations aimed at:
- Providing timely decisions for all Veterans – regardless of gender, language, or other factors;
- Standardizing Service Standard Start Dates so that turnaround times can be meaningfully reported;
- Triaging applications based on need;
- Eliminating the negative consequences of delays; and
- Providing more information to applicants about expected turnaround times, reasons for delay, and incomplete applications.
Turnaround times will continue to be a top complaint of Veterans and one of the biggest challenges faced by VAC until significant changes can be made more broadly to processes, systems, and approaches to service delivery. By implementing the recommendations made in this report, VAC will be able to better meet the needs of all Veterans and their families in a timely manner.
Introduction
From calls to our frontline to town hall and stakeholder meetings across the country, the complaint the OVO hears most often from Veterans and their families is about lengthy and unreasonable delays for disability benefit decisions. These delays have been the subject of countless news stories and social media posts. In fiscal year 2016-17, we received 208 complaints related to disability benefit turnaround times; in 2017-18 we received 274 complaints. These numbers represent 18% and 20% respectively of the total number of complaints received.
A Veteran recently commented: "
100% of my claims take longer than the 16 weeks, and they haven't even been close to that target. If they can't make 16 weeks, give us a reasonable target they can meet. I am tired of excuses and so are most of the Veterans I talk to."Footnote 1
This number of complaints is not surprising given the impact of wait times for decisions. A favourable disability benefit decision can be a gateway to other benefits and services such as access to medical treatment for service-related injuries and a variety of benefits that help provide financial security to ill and injured Veterans. Lengthy wait times and a lack of transparency can also negatively impact the trust relationship between Veterans and the department meant to serve them. We hear that frustration is further amplified when expectations set by VAC are consistently unmet.
The OVO defines fairness as an outcome that can be measured in terms of adequacy, sufficiency, and accessibility:
- Are adequate benefits in place to support Veterans?
- Are those benefits sufficient to meet the needs of Veterans and their families?
- Are Veterans and family members able to access those benefits easily and quickly?
In order to be treated fairly, Veterans need to receive timely decisions and access to disability benefits. This report focuses on the fairness principle of accessibility, including whether actions to mitigate existing delays are equitable and based on need.
Definitions

Who
Who
War service Veterans
Served during WWII or the Korean War
Canadian Armed Forces (CAF) Veterans
Served any time after 1947, except during the Korean War
Still serving CAF members
Members of the Canadian Armed Forces who have not yet released and are receiving a salary and access to healthcare from the CAF

What
What
Disability Benefit
A financial payment provided to an individual with a service-related disability. There are two main components to a disability benefit decision:
-
Entititlement (expressed in fifths):
The extent to which a condition is related to service. Entitlement grants access to treatment benefits.
-
Assessment (expressed as a percentage):
The degree of impairment from the disability.
How
How
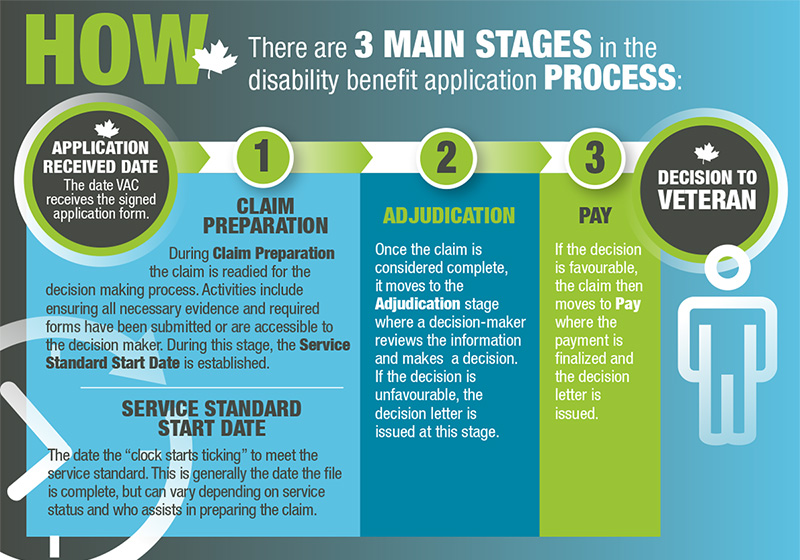
There are 3 main stages in the disability benefit application process
Application received date
The date VAC receives the signed application form
-
Claim preparation
During Claim Preparation the claim is readied for the decision making process. Activities include ensuring all necessary evidence and required forms have been submitted or are accessible to the decision maker. During this stage, the Service Standard Start Date is established.
Service Standard Start Date
The date the "clock start ticking" to meet the service standard. This is generally the date the file is complete, but can vary depending on service status and who assists in preparing the claim.
-
Adjudication
Once the claim is considered complete, it moves to the Adjudication stage where a decision-maker reviews the information and makes a decision. If the decision is unfavourable, the decision letter is issued at this stage.
-
Pay
If the decision is favourable, the claim then moves to Pay where the payment is finalized and the decision letter is issued.
Decision to Veteran
Methodology
A Veteran-centric approach was adopted to learn about the delays Veterans are experiencing when waiting for disability benefit decisions. This type of review allowed us to analyze the information from the Veteran’s perspective and to make recommendations that improve transparency, timeliness of access, and the meeting of individual needs. To do this, we:
- reviewed all elements of the process, including claim preparation, adjudication, and payment;
- reviewed Pension Act and Veterans Well-being Act legislation and Veterans Health Care Regulations;
- reviewed all applicable and available VAC documents, including business processes, directives, workflows, and guidelines. Publicly available documents included program policies and departmental reports;
- conducted detailed analyses of 1,050 completed disability benefit first application files, in two random samples, from fiscal year 2016-17:
- Scope was limited to Veterans and still-serving Canadian Armed Forces (CAF) members (RCMP was excluded) to control for differences in types of service and timelines for accessing relevant health records.
- Reassessments, Departmental Reviews, and applications submitted to the Veterans Review and Appeal Board (VRAB) were excluded to control for different service standards and business processes.Footnote 2
- Only files with completed decisions were reviewed in order to ensure each claim included all components of the process.
- Each file was analyzed, including calculating timeframes spent at each stage of the process, examining client notes and work items for information on delays, and tracking demographic information such as language, age, and gender.
- The first random file sample included 750 decisions. Analysis of this sample led us to request a second random file sample of 300 decisions using more restricted parameters (only CAF Veterans and still-serving members) to gain a clearer picture of the initial trends we identified from the first sample.
- analyzed general statistical information on applications submitted by the entire client population during fiscal year 2016-17; and,
- observed and consulted staff at on-site visits to the Dartmouth Disability Benefit Unit and Charlottetown Veterans Affairs Canada Head Office to become familiar with the claim preparation, adjudication, and pay stages of the disability benefit application process.
Initial File Sample Review
We began our review by conducting an in-depth analysis of 750 randomly selected files. We reviewed each step of the process from submission of an application to decision and payment, if applicable, and identified the degree to which VAC’s 16-week service standard was met and for whom.
War Service (WS) Applications
The majority of these decisions were issued within the service standard of 16 weeks.
Table 1: Percentage of applications meeting the 16-week service standard by language of applicant
| Language of Applicant | % (#) within 16 Week Service Standard |
|---|---|
| English | 99% (99/100) |
| French | 91% (58/64) |
Red Zone Applications
Red Zone applications are triaged for priority adjudication due to medical risk, and less often, financial risk.
When an application is identified as “Red Zone”Footnote 3, a Red Zone start date is added once all information required to make a decision has been received.Footnote 4 Red Zone is an internal process that may or may not require a date change if it is determined later that more information is needed to make a decision. VAC’s service standard for medical risk – palliative applications is seven business days. For other medical and financial Red Zone applications, the service standard is 10 business days, but because the Red Zone start date is variable and can be determined at any stage (from claim preparation to the payment stage), it is difficult to determine if Red Zone decisions were being issued within seven or 10 days of being identified as Red Zone. However, we are able to confirm that the vast majority (97%) of the 100 Red Zone applications in our sample, expedited due to unmet health needs or financial distress, were completed within 16 weeks of the Service Standard Start Date.
The Service Standard Start Date is the date the “clock starts ticking” to meet the service standard.
To get a better sense of whether Red Zone claims were in fact being completed in the seven or 10 day service standard, we requested the average turnaround times for all 2016-17 Red Zone claims from VAC. They provided the following statistics:
Table 2: Average turnaround time for Red Zone claim typesFootnote 5
| Red Zone Type | Average Turnaround Times |
|---|---|
| Medical Risk Palliative | 7.47 days |
| Medical Risk Other | 7.80 days |
| Unmet Health Need | 11.73 days |
| Financial Distress | 15.96 days |
CAF Still-Serving and CAF Veterans – not Red Zone
When we looked at CAF still-serving members and CAF Veteran applications where the claim was not Red Zone, we found that a majority (70% or 266/378) were delayed beyond the 16-week service standard.Footnote 6
Figure 1: CAF Still-Serving and CAF Veteran claims completed within and beyond the service standard
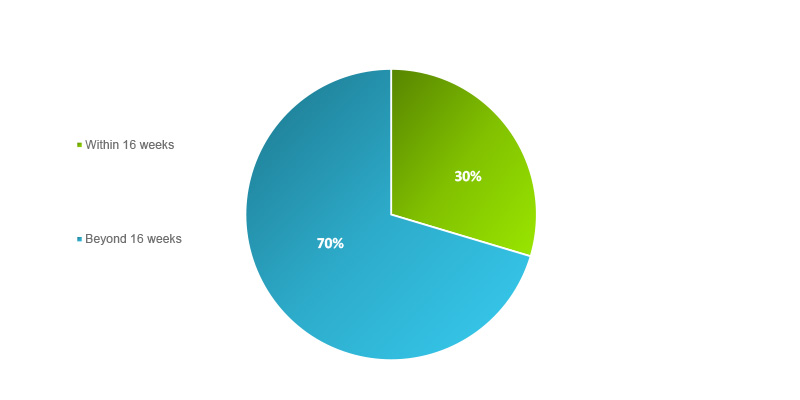
The average turnaround time for this group was 23 weeks from the Service Standard Start Date and a quarter of these applications took more than double the service standard (i.e. 32 weeks or more). When looking into those applications that took the longest, we noticed that Francophone applications were disproportionately present (approximately 15% of all applications are from Francophone clients).Footnote 7
- 63% (60/96) of applications taking 32 weeks or more were from Francophone clients.
- 20 decisions (5% of our sample) took more than 43 weeks to complete, and 90% (18/20) of these were submitted by Francophone clients.
- All decisions that took longer than one year (four in total) were submitted by Francophone clients.
Figure 2: Applications that took the longest
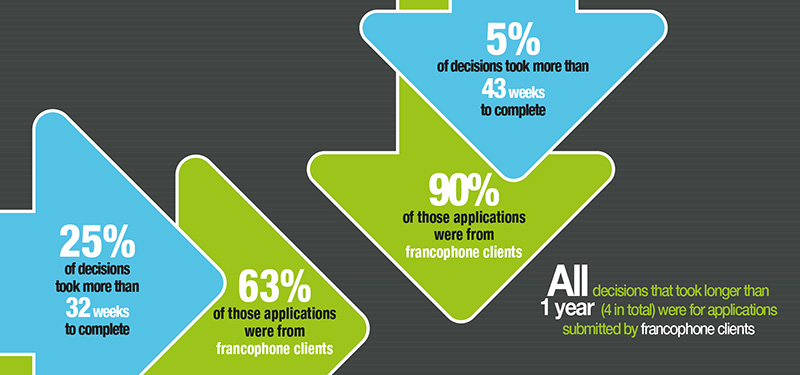
Applications that took the longest
Applications that took the longest
- 25% of decisions took more than 32 weeks to complete
- 63% of those applications were from francophone clients
- 5% of decisions took more than 43 weeks to complete
- 90% of those applications were from francophone clients
- All decisions that took longer than 1 year (4 in total) were for applications submitted by francophone clients
Our analysis of this initial file sample suggested that War Service and Red Zone applications were processed in a timely manner. This is good news. The problem, though, is that reports on actual turnaround times include these prioritized applications, dramatically lowering the average timeframe. This makes it difficult to determine how long Veterans wait when their applications are not prioritized. It also makes it difficult to set expectations accordingly.
In effect, VAC publicly communicates that their Service Standard (i.e. the timeframe clients can expect between the Service Standard Start Date and the date a decision is received) is 16 weeks. However, VAC reports that it only met this target 43% of the time in 2016-17.Footnote 8 Because this 43% includes Red Zone applications, the Service Standard set by the department and actual turnaround times for regular, non-prioritized claims are not transparent.
Figure 3: Measuring performance
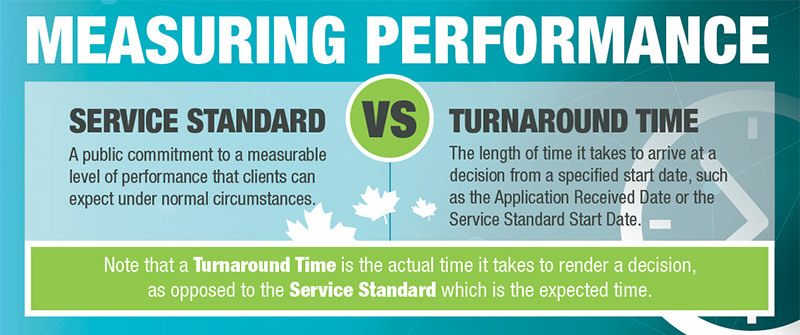
Measuring performance
| Measuring performance | ||
|---|---|---|
| Service Standard | VS | Turnaround Time |
| A public commitment to a measurable level of performance that clients can expect under normal circumstances. | The lenght of time it takes to arrive at a decision from a specified start date, such as the Application Received Date or the Service Standard Stard Date. | |
Note that a Turnaround Time is the actual time it takes to render a decision, as opposed to the Service Standard which is the expected time.
As a result, we requested a second file sample, limited to only applications from CAF still-serving members and CAF Veteran clients, in order to look further into areas of concern identified in the first sample, such as delays for Francophone clients. This second file sample forms the basis of the rest of our review.
Second File Sample Review
To ensure we were comparing apples to apples, we requested a second random sample that excluded applications submitted by War Service Veterans and those expedited under the Red Zone process. All files in the second sample were from CAF Veterans and still-serving members. This random sample included 300 files completed during fiscal year 2016-17.Footnote 9
In this sample, the average turnaround time from the Service Standard Start Date was 29 weeks; however, from the Application Received Date, individuals waited 31 weeks on average for a decision.
Figure 4: Turnaround time perspectives
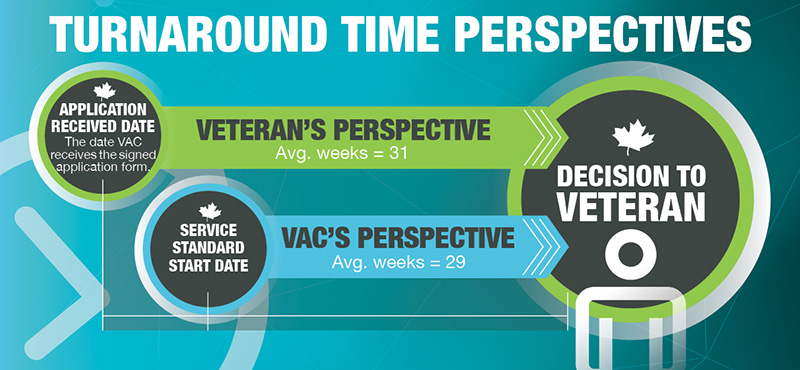
Turnaround time perspectives
Turnaround time perspectives
Veteran’s Perspective:
Application Received Date (The date VAC receives the signed application form) to Decision to Veteran = 31 weeks on average
VAC’s Perspective:
Service Standard Start Date to Decision to Veteran = 29 weeks on average
The application and decision-making processes are not clearly or transparently communicated. As a result, Veterans can feel like they are waiting longer because they are not aware that the clock starts ticking only once their application is considered complete by VAC.
At an OVO town hall a Veteran recently commented: "
The fact that the time doesn't start until VAC decides it starts means the 16-week metric is meaningless…"
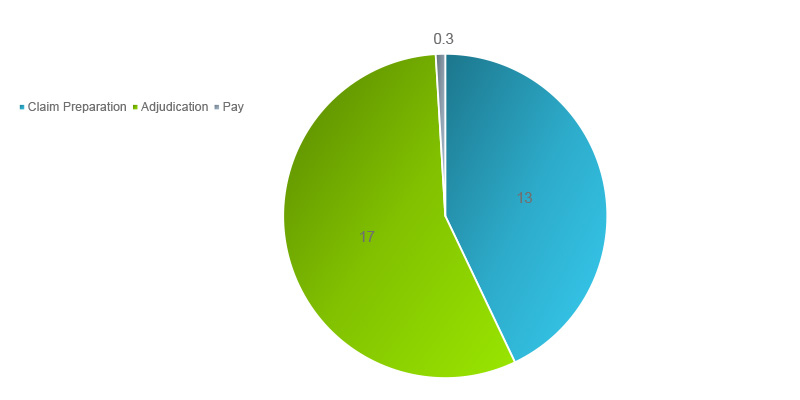
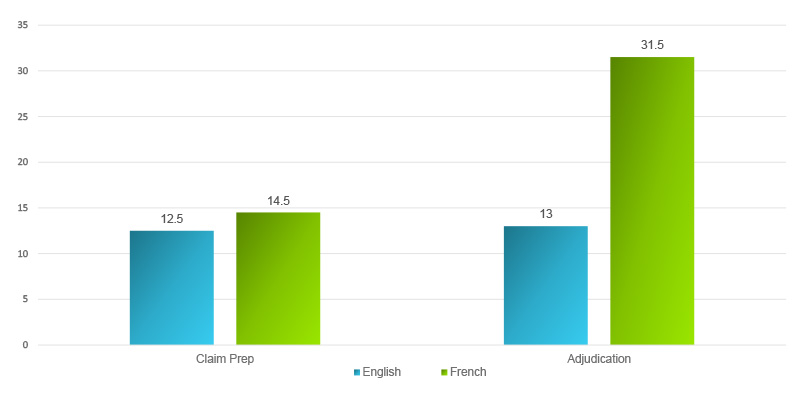
The graph below (Figure 5) shows that the applications in the sample spent an average of 13 weeks in Claim Preparation and 17 weeks in Adjudication.Footnote 10 Once claims were sent to Pay, it only took an average of two days to issue the payment, send the letter, and complete the decision. The Service Standard sets expectations that a decision will take 16 weeks, but 13 weeks often goes by before an application even reaches the decision-making stage.
Figure 5: Average number of weeks an application spends in each processing stage
Findings: Inequitable Wait Times
Our analysis revealed that some groups of applicants wait longer than others and that these differences appear to be arbitrary and not based on a difference in needs.
Wait times were often unduly affected by:
- The first official language of the applicant.
- The gender of the applicant.
- How the Service Standard Start Date is determined.
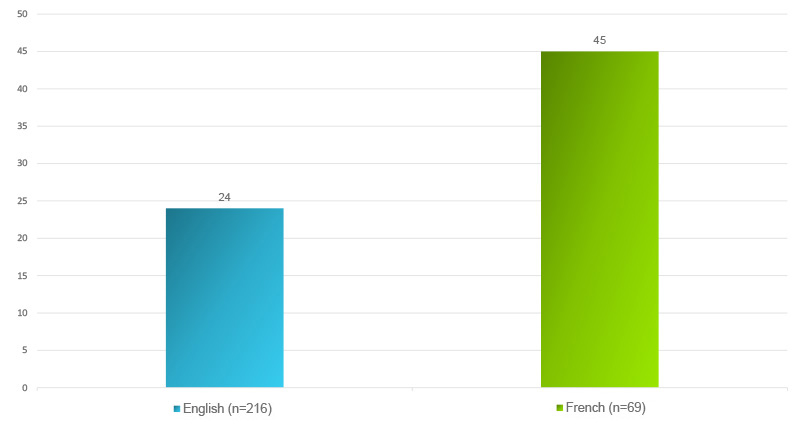
Francophone applicants waited longer
In the file sample, Anglophone applicants waited 24 weeks, on average, for a decision. On the other hand, Francophone applicants waited an average of 45 weeks. This constituted a substantial difference in wait time: 21 weeks, or approximately five months.
Figure 6: Average turnaround time (in weeks) by first official language of applicant
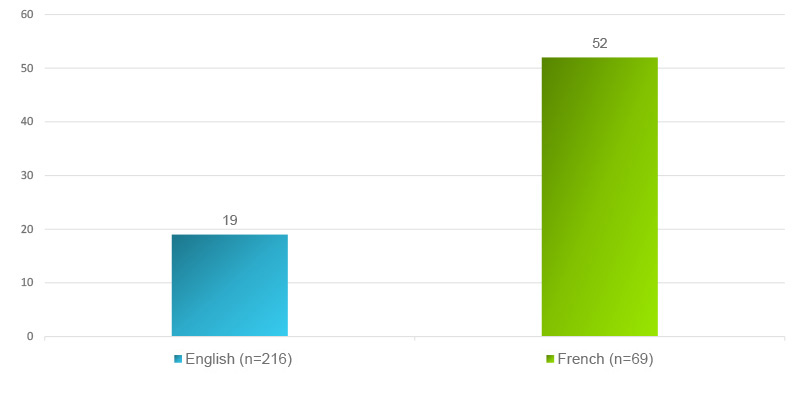
To eliminate the possible influence of outliers on our average calculation, we compared the median timeframes and found that the difference was even larger.Footnote 11 The median time to issue a decision for Anglophone clients was 19 weeks, versus 52 weeks for Francophone clients, which is a difference of 33 weeks. Therefore, half of all Francophone applications in our sample took one year or longer to complete.
Figure 7: Median turnaround time (in weeks) by first official language of applicant
Next, we compared Francophone and Anglophone turnaround times in the graph below (Figure 8) and found that the majority of Anglophone applications (noted in grey) were completed in under 20 weeks. Meanwhile, the majority of Francophone applications (noted in blue) took over 48 weeks to complete.Footnote 12
Figure 8: Distribution of turnaround times for English and French applications
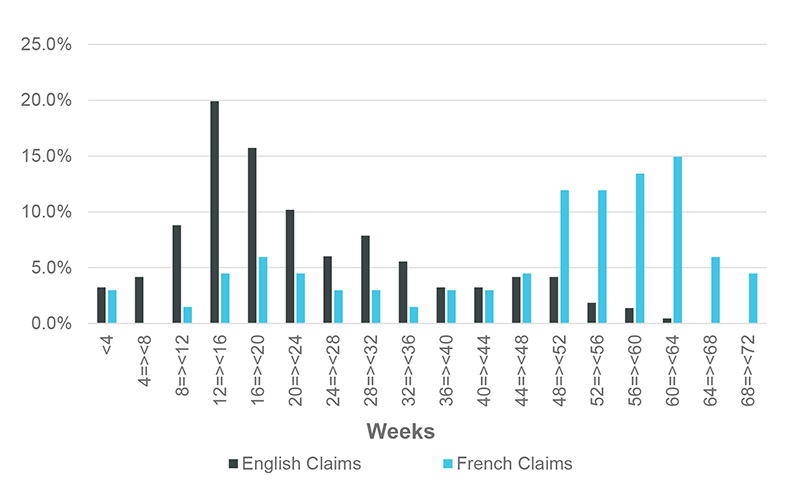
As of December 2017, there were 2,771 first applications pending with a Service Standard Start Date in the previous fiscal year (2016-17). Of these applications, 42% were from Francophone clients, yet only 15% of all applications submitted in 2016-17 were from Francophones.Footnote 13
To help determine why Francophones appeared to wait much longer than Anglophones, we compared how long their applications spent in each stage of the process. The following graph (Figure 9) shows that Francophone applications spent only slightly longer than Anglophone applications in the claim preparation stage; however, the delay Francophone clients experience appears to result from delays during the adjudication stage.
Figure 9: Turnaround time (in weeks) by stage and language of application
Pierre and Peter applied for an obstructive sleep apnea disability benefit. Pierre submitted his application in French, and Peter submitted his in English. Pierre waited 45 weeks for a decision, whereas Peter waited 24 weeks. Both needed coverage to pay for their continuous positive airway pressure (CPAP) machines and both waited too long for their decisions. Despite submitting very similar applications at the same time, Pierre had to wait over five months longer than Peter to obtain his CPAP machine.
15% of all applications submitted in 2016-17 were from Francophones.
VAC advised that 18% of nurse adjudicators have the language proficiency required to make decisions on Francophone applications, alongside 28% of benefit adjudicators, who work on less complex files.Footnote 14 Thus, it appears that the resources are in place to meet this demand, but there is still a gap. It is unclear whether staffing resources are sufficient or if those with the most capability in French are being assigned, on a priority basis, to Francophone claims.
Women waited longer
Female clients in our sample waited on average 32 weeks – 3.6 weeks longer than male clients who waited 28 weeks on average. The median time to issue a decision was 23 weeks for male clients and 31 weeks for female clients – a difference of eight weeks.Footnote 15
We compared applications submitted by females with those submitted by males in the following graph (Figure 10). We found that 42% of female clients (blue) waited over 40 weeks for a decision, while only 26% of male clients (grey) waited that long.Footnote 16
Figure 10: Distribution of turnaround times for male and female applications
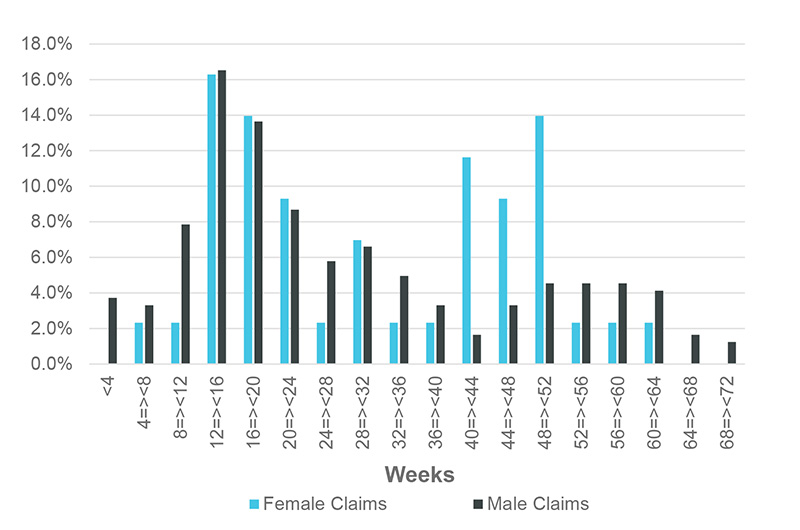
It is possible that systemic issues are impacting wait times for female Veterans. For instance, women and men may be employed at different rates in certain military occupations, potentially leading to different medical conditions. A review of the conditions that follow the streamlined models would be beneficial to determine if they may be more reflective of injuries sustained by men or in male-dominated professions.Footnote 17
The Government of Canada expects departments to provide services to all Canadians in an equitable manner. To do so it uses a variety of policy instruments such as the Treasury Board Policy on Official LanguagesFootnote 18 and the mainstreaming of Gender-Based Analysis + tools in the development of policies and programs.Footnote 19 Our review leads us to be concerned that the diversity of applicants may not have been fully considered during the development of decision-making tools and business processes.
Recommendation 1: Provide equitable access to timely decisions regardless of factors such as the applicant’s gender and language.
Service Standard Start Date inconsistencies
VAC uses a first-in first-out queue based on the Service Standard Start Date,Footnote 20 which is the first day in the 16-week countdown to the decision’s due date, based on the service standard. A Service Standard Start Date that is after January 1 will have a due date after April 23. Accordingly, all else being equal, such as the date of application, the Service Standard Start Date determination can be a significant factor in determining when VAC begins to review the application and, as a result, how long an applicant waits for a decision.
A first-in first-out queue means that the earlier the ‘clock starts ticking’, the sooner the decision becomes due. Applications have a different Service Standard Start Date depending on two factors: service status (still-serving or Veteran); and who prepares the claim (VAC or the Royal Canadian Legion (RCL)).
Table 3: Differences in Service Standard Start Date Determination
| Who Prepares the Claim | Service Status | Determination of Service Standard Start Date |
|---|---|---|
| VAC | Still-serving member | The Service Standard Start Date is the date VAC receives a signed application form, identity and consent forms, provided that there is a diagnosis in the applicant’s Service Health Records.Footnote 21 VAC absorbs any time it takes to obtain Service Health Records and other medical documentation from the CAF. Therefore, the Service Standard Start Date is usually closer to the date the application is submitted.Footnote 22 |
| Veteran | The Service Standard Start Date is the date that VAC has received a fully completed application form and all supporting documents from the applicant. This would include: consent, profile and identity forms, the application form, and any required supporting medical documentation such as medical questionnaire(s), audiogram, x-ray, specialist report, Member Personnel Record Resume, CF98, hazardous incident report, etc.Footnote 23 | |
| Royal Canadian Legion (RCL) | Still-serving member or Veteran | The Service Standard Start Date is the date the claim is received by VAC Head Office.Footnote 24 Because the RCL completes the claim preparation portion of the process before sending it to Head Office, the Service Standard Start Date can be much later than the date all required information has been submitted by the applicant. |
As shown in Figure 11 below, these different processes are not transparent to applicants. They are not advised that there is a difference in how their Service Standard Start Date is calculated – depending on the definition of “complete”, whether or not they are still-serving, and who prepares the claim – all of which can impact their place in the queue and ultimately when they receive their decision.
Figure 11: Disability benefit queue
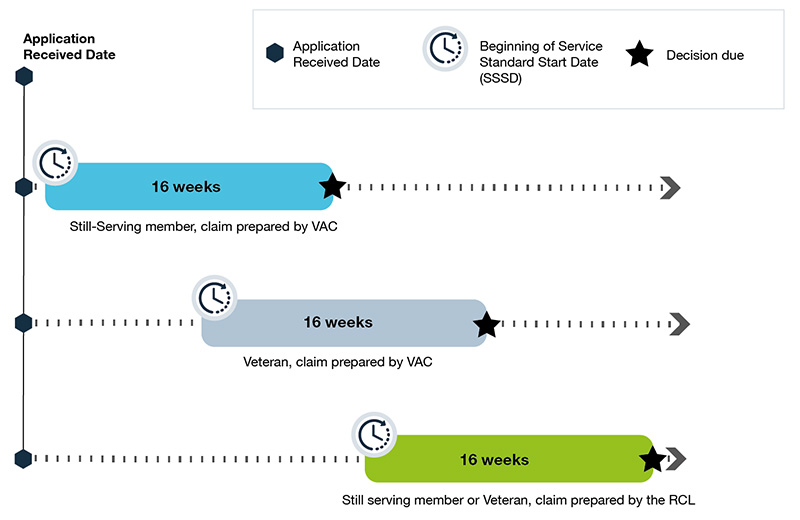
Disability benefit queue
Timelines with the same Application Received Date for each:
Still-serving member, claim prepared by VAC
Earliest Service Standard Start Date, earliest decision due date
Veteran, claim prepared by VAC
Service Standard Start date and decision due dates are later than Still-serving members
Still serving member or Veteran, claim prepared by the RCL
Latest Service Standard Start Date and decision due date
Service Standard Start Dates are important because they are used as a basis to measure whether or not VAC is meeting its published service standards. Inconsistent Service Standard Start Dates mean that VAC is not really using a first-in first-out queue, and that reports from VAC on average turnaround times are inaccurate and misleading. All else being equal (i.e. similar conditions and the absence of health or financial risk), those with the same Service Standard Start Date should have their claims processed in the same amount of time. Accurate, consistent, and well-communicated Service Standard Start Dates are needed to ensure all Veterans are treated fairly and to enable VAC to more accurately report on turnaround times for decisions.
Natalie applied for a Disability Award for PTSD in June 2016. She was still-serving, and the diagnosis was available in her CAF Service Health Records. The 16-week Service Standard Start Date began on the date she applied. As a still-serving member of the CAF, Natalie was receiving mental health treatment, prescription drug coverage, and a full salary.
At the same time, Amy also applied for a Disability Award for the same condition. She was released from the CAF and was working full-time. She was prescribed expensive treatment for her PTSD, and she struggled to balance her treatment costs while making ends meet. In her case, the clock did not start ticking on her application until VAC considered it complete, including all necessary documentation from her doctor and specialist. This took an extra four weeks to obtain and submit.
Amy arguably has a greater need than Natalie, but received a decision four weeks later because of the difference in Service Standard Start Dates.
Recommendation 2: Standardize Service Standard Start Dates to improve transparency and equity and facilitate accurate performance reporting.
Findings: Opportunities for Needs-Based Triage
Every individual who submits a disability application has a unique set of needs that could be addressed with a favourable disability benefit decision. The level of need depends on a variety of factors such as health status, employment status, financial resources and age, among others. Our analysis points toward opportunities for VAC to improve the way it triages applications in order to achieve better outcomes for Veterans depending on their level of need.
How VAC triages
VAC triages applications when a Veteran meets its “Red Zone” criteria for one of the following categories:
- Medical risk
- Unmet health need related to claimed condition
- Financial distress
Veterans who submit a complete application and who are over the age of 80 are automatically ‘Red Zoned’ and placed at the front of the queue.Footnote 25 A Veteran who does not meet this age criteria, but who may be palliative or facing a high level of medical risk, experiencing an unmet health need related to the claimed condition, or experiencing severe financial distress, can request that VAC expedite their claim.
Streamlined Decision-Making Models have been developed for certain conditions that have a clear link to service, such as hearing loss and tinnitus, PTSD, and some musculoskeletal conditions.
VAC also triages based on condition.Footnote 26 Certain conditions, such as hearing loss and tinnitus, are processed through streamlined decision-making models. If the condition meets the criteria in the model, the decision may be made more quickly. If the claim is more complex – maybe because the link to service is less clear – or if it does not meet the requirements of the model, it goes through the conventional adjudication process. An example of a more complex condition-type would be a disease such as cancer or diabetes.
Opportunities for improvement
The automatic “Red Zoning” of applications submitted by elderly Veterans is a proactive approach to triaging. It helps ensure those who face greater risks to their health receive their decision as soon as possible.
In most other cases, VAC reactively triages applications submitted by applicants who are at greater medical or financial risk when the client expresses and proves this risk to the department.
- Red Zone processes are not advertised by VAC, and criteria are not publicly available.
- Whether or not a Veteran with an unmet health need is identified by VAC and triaged accordingly depends on if the Veteran has alerted VAC about their situation, or has been advised to request Red Zone triaging by our Office, by an advocate, or by a fellow Veteran (i.e., through word-of-mouth).
In 2016, Jim, age 35, and Tom, age 85, both applied for disability benefits for osteoarthritis for their knees. Because Tom is 85, his application was automatically processed as a priority and he received his decision in seven weeks. Jim knew his treatment would not be covered unless he received a favourable decision from VAC. He decided to wait, forgoing the treatment. Nobody told him he could request to have his application expedited due to an unmet health need. Jim waited 23 weeks for his decision.
There are clear opportunities to improve triaging and better communicate available priority queues to ensure that no Veteran goes without needed benefits while they wait for a decision. For instance, a client’s service status – whether still serving, in the process of releasing, or already released – can indicate the likelihood of an unmet service-related medical need.
Still-serving, full time members of the CAF have access to treatment for medical conditions and they receive a regular salary. Until a still-serving member begins the process for release, they are the least likely to have an unmet need resulting from a service-related medical condition.
Veterans who have released can no longer access medical treatment from the CAF. This means that Veterans and releasing members are more likely to have an unmet health need than still-serving CAF members without a release date.Footnote 27
Members releasing from the CAF may have an increased need. If they release prior to a decision, they could experience a gap in health care coverage for their service-related conditions.Footnote 28
In 18 of the files we analyzed, the client had released while their application was in progress. Despite previous recommendations from the OVO to ensure that transitioning members have all VAC benefits in place at time of release, the department does not track or triage applications submitted by members with a release date to ensure they do not experience a gap in medical coverage for their service-related conditions.Footnote 29
VAC does not track the release date of still-serving members who apply for departmental benefits.
For transparency purposes, we recommend that Service Standard Start Dates be consistent and clearly communicated. Service Standards (the expected timeframe for a decision) do not, however, need to be uniform for all scenarios. VAC could meet the most pressing health care needs of its clients by establishing different service standards based on need, linked to service status or access to treatment. For instance, still-serving regular force members and Veterans who already have comprehensive coverage from VAC do not need the treatment benefits that result from a favourable decision; therefore, they could have a longer service standard.Footnote 30 Applications should also be triaged to ensure releasing members do not experience a gap in treatment benefits upon release from the CAF.
This approach requires a transparent, well thought out communications plan. It should advise clients exactly what the different service standards are, where their application fits in the process, and how long their individual decision will take. Clients should not be treated the same when their requirements are different. VAC needs to do more to ensure that the timeliness of decisions is equitable – i.e., that the turnaround time for a decision is influenced more by the needs of the applicant.
Recommendation 3: Triage applications upon receipt based on health and financial need.
Findings: Consequences of Delays
Delays are a serious issue when they impact timely access to compensation and other benefits, including access to health care treatment for illness and injury.
Equitable access to health care under the Veterans Well-being Act
Recently, a Veteran explained: "
I'm at the 19-week mark since my application was accepted. It's been at Step 3 for the past two months… I suffer from PTSD, have exhausted my employee benefits (I'm civilian now) and spent as much as I can from my personal finances on therapy, only to have to stop treatment until (hopefully) my application is approved. I can't imagine waiting another year."
Access to treatment benefits is inequitable, for it depends on whether eligibility is granted through disability entitlement under the Pension Act or the Veterans Well-being Act. The Veterans Health Care Regulations provide retroactive access to the reimbursement of health care treatment costs 90 days prior to the date of application for a favourable Disability Pension. On the other hand, a favourable Disability Award only allows access to reimbursement from the date of the decision with no access to any retroactive reimbursement.Footnote 31 We identified this issue in our 2012 “Veterans' Right to Fair Adjudication” report,Footnote 32 and repeatedly since then to VAC senior officials and the Minister of Veterans Affairs.
In January 2006, Philip applied for a Disability Pension for broken teeth under the Pension Act. He waited 20 weeks for a decision, and during that time, he paid for dental care out of his own pocket. VAC found that his condition was related to his service, and the decision was favourable! Philip saved his receipts and was reimbursed by VAC for any expenses he incurred up to three months before he applied.
Julie submitted her application for the same condition in April 2006 (under the New Veterans Charter). Unfortunately for her, none of her expenses prior to the decision date are eligible for reimbursement by VAC.
This inequity is further exacerbated by delays in the processing of claims. Delays mean that some Veterans may have to shoulder the financial burden of treating a condition caused by service for sometimes almost a year while they wait for a pending decision. Worse still, these Veterans may delay treatment and potentially aggravate a service-related medical condition if coverage is not available elsewhere.
Recommendation 4: Reimburse all Veterans’ health care expenses for approved claimed conditions 90 days prior to their date of application.
Fairness for those who pass away while application is in progress
When a Veteran dies while their application is in progress, the application can continue if a surviving spouse/common-law partner or dependent child is identified.Footnote 33 When a single client with no dependent child dies while their application is in progress, VAC has no authority to pay the disability benefit to the estate, and consequently the application is withdrawn. Both the Pension Act under Section 48(2) and the Veterans Well-being Act under Section 50(2) protect dependents, but not the estate of a single CAF member or Veteran with no dependents.Footnote 34 Since April 2000, there have been 5,173 Veterans who have died with a disability benefit first application in progress and 646 (or 12%) of these did not proceed.Footnote 35
Gillian and Bernard both applied for a disability benefit and passed away while their respective applications were in progress. Because Gillian had a dependent child, VAC continued to adjudicate the application and paid the award to Gillian’s survivor. Bernard, on the other hand, had neither a dependent child nor a surviving spouse. He was, however, the primary caregiver for his elderly parents who were the beneficiaries of his estate. Because Bernard had no surviving spouse or dependent children, his claim was withdrawn.
As noted previously in the OVO’s report Fair Compensation to Veterans and their Survivors for Pain and Suffering, the Disability Award and the Disability Pension are “intended to recognize sacrifice and compensate for the pain and suffering of a service-related disability for all members and Veterans”.Footnote 36 It is not fair that, due to delays outside the control of the applicant, there may be instances when an application dies with the claimant.
Notably, as of April 1, 2018, VAC has the authority to make payment to an estate when, at the time an applicant passed away, a favourable decision had been made but not yet paid out. This has no impact on applications in progress – i.e. where the applicant was waiting for the decision at the time of death.
Recommendation 5: When a Veteran dies with a disability benefit application in progress, continue to process the application and permit payment to the estate if the decision is favourable.
Findings: Communication and Transparency
Until VAC can provide timelier decisions on a consistent basis, more can and should be done to keep Veterans informed about the process and what to expect.
Upfront proactive communications
We have heard from Veterans that not only are they frustrated with delays in the processing of their applications, they are also kept in the dark about the status of their applications, when they can reasonably expect a decision, and what the decision entails.
A Veteran recently commented: "
Let’s be upfront and honest. Most Veterans can work with the truth and may have made other financial commitments based on the expected processing time."
VAC has information that it could proactively share with Veterans on its website and through their My VAC Account. This could include the average turnaround times for common conditions. Further, VAC has an internal turnaround time report that already includes this information, which could be shared publicly.
Information currently provided on My VAC Account
| Step 1 | VAC received your application form. We are awaiting additional information in support of your claim. |
|---|---|
| Step 2 | We are reviewing all of the information obtained in support of your claim. |
| Step 3 | Your claim is currently at the decision-making level. All your supporting documentation was received on [date]. You should expect a decision letter within 16 weeks of this date. |
My VAC Account advises Veterans whether their claim has passed from Stage 1, 2, or 3. Currently, this information is not detailed enough to be meaningful (see information provided on My VAC Account below). More specific details could be provided to the Veteran through My VAC Account.
Veterans should be informed throughout the entire application process of all possible outcomes, not just favourable and unfavourable. For instance, some conditions are more likely than others to result in an initial 10% minimum assessment – requiring a reassessment at a later date, usually when the condition has stabilized. Veterans should be informed that this initial assessment is a possibility in these cases.
Recommendation 6: Provide each applicant with an individualized, expected turnaround time for their application, and inform them if the decision will be delayed and why.
Incomplete applications
VAC spends a substantial amount of time following up with clients and doctors when incomplete applications are submitted. For example, when a hearing loss claim is submitted without the required audiogram, VAC staff will often repeatedly follow-up with the client and/or medical providers to obtain the missing information. This follow up activity may seem like excellent customer service, but in a backlog situation it may not be the best use of time.Footnote 37
VAC’s Audit and Evaluation Division found in their 2015 Evaluation of Disability Benefits report that when an incomplete application is received, “…it takes on average an additional 35 days to begin processing”.Footnote 38 While staff chase after incomplete applications, completed applications are waiting to be processed. Clearer instructions and tools to help applicants determine what exactly is required could facilitate the submission of complete applications, and assist with workload management. Furthermore, upon receipt of applications, they should be reviewed for completeness, and, if incomplete, returned with an explanation, as quickly as possible. This would bring VAC in line with other government services such as Canada’s Passport Program.
Recommendation 7: Provide clients with a checklist of all required documents on the application form and, upon receipt, immediately return applications if required documents are missing.
Conclusion
VAC reports that they are receiving an increased number of applications compared to previous years. This backlog may be worsened by the upcoming implementation of Pension for Life benefits planned for early 2019. Now is the time to ensure that the planning and resources required to deliver disability benefits, both equitably and in a timely manner, are in place.
Lengthy turnaround times for disability benefit decisions is about more than monetary compensation for pain and suffering. Many applicants have unmet health needs that can be exacerbated by waiting for adequate treatment.Footnote 39 Resources should be allocated to ensure that those with the highest level of need receive their decisions before those whose health requirements are already met. While triaging applications based on whether they are ‘simple’ or ‘complex’ can improve overall efficiency, we caution VAC to stay focused on the needs of applicants and to ensure that simple/complex triaging does not inadvertently cause longer wait times for those whose claim may be complex, but who may have greater health needs.
Future spending to address the backlog of disability benefit applications needs to address equity and efficiency by ensuring appropriate resources are in place and by leveraging available technological advances. New funding presents an important opportunity for targeted spending that focuses on long-term, proactive solutions to achieve equitable results that meet the needs of all Veterans who are dealing with a service-related illness or injury.
Turnaround times will continue to be a top complaint of Veterans and one of the biggest challenges faced by VAC until significant changes can be made more broadly to processes, systems and approaches to service delivery. While it is acknowledged that some recommendations may take more time to implement, others can be addressed in short order, and we will continue to monitor progress.
Implementing these recommendations will ensure that:
- All Veterans receive timely decisions – regardless of gender, language or other factors.
- Applications are triaged based on need.
- The negative consequences of delays are eliminated.
- More accurate and transparent information is provided to Veterans about expected turnaround times, reasons for delay and incomplete applications.
Our Veterans expect no less.
